
American Heart Association President Suffers Heart Attack at 52
Dr. Mercola
In the health paradox of the year, 52-year-old cardiologist John Warner, president of the American Heart Association (AHA), recently suffered a heart attack in the middle of a health conference.1,2 In a statement, the association reported Warner was in stable condition after having a stent placed to open a blocked artery. Part of Warner’s speech at the Scientific Sessions conference in Anaheim, California, centered around his own family’s struggle with heart disease.
"After my son was born and we were introducing him to his extended family, I realized something very disturbing: There were no old men on either side of my family. None. All the branches of our family tree cut short by cardiovascular disease," Warner said in his speech.3
“Together we can make sure old men and old women are regulars at family reunions, that people live long enough and healthy enough to enjoy walks and fishing trips with their grandchildren and maybe even their great-grandchildren. In other words, I look forward to a future where … children grow up surrounded by so many healthy, beloved, elderly relatives that they couldn't imagine life any other way.”
The AHA’s CEO, Nancy Brown, said in a statement:4 “John wanted to reinforce that this incident underscores the important message that he left us with in his presidential address … that much progress has been made, but much remains to be done.”
Many AHA Recommendations Worsen Heart Health
In all likelihood, Warner followed AHA recommendations, many of which are actually recipes for heart disease disaster. Of the foods scientifically proven to cause heart disease and clogged arteries, excess sugar and industrially processed omega-6 vegetable oils, found in nearly all processed foods, compete for space at the top the list. And what kinds of foods does the AHA recommend to protect your heart?
Not only does it support ample grain consumption, it also recommends eating harmful fats such as canola, corn, soybean and sunflower oil.5 “Blends or combinations of these oils, often sold under the name ‘vegetable oil,’ and cooking sprays made from these oils are also good choices,” the AHA says. Meanwhile, the association still insists saturated fats are to be avoided.
Just this past summer the AHA shocked health experts around the world by sending out a worldwide advisory6 saying saturated fats such as butter and coconut oil should be avoided to cut your risk of heart disease, and that replacing these fats with margarine and vegetable oil might cut your heart disease risk by as much as 30 percent. Overall, the AHA recommends limiting your daily saturated fat intake to 6 percent of daily calories or less.7
This is as backward as it gets, and if Warner was following this long-outdated advice, it’s no wonder he suffered a heart attack. In fact, it is to be expected. As noted by American science writer Gary Taubes in his extensive rebuttal to the AHA’s advisory,8 with this document, the AHA reveals its longstanding prejudice — and the method by which it reaches its flawed conclusions.
In short, the AHA simply excluded any and all contrary evidence. After this methodical cherry-picking, they were left with just four clinical trials published in the 1960s and early ‘70s — the eras when the low-fat myth was born and grew to take hold. The problem is nutritional science has made significant strides since then, and a number of significant studies have firmly disproven the hypothesis that saturated fat causes heart disease, finding no association whatsoever.
In related news, the AHA recently issued new guidelines on blood pressure,9 moving the goal post for heart health yet again. Now you’re considered hypertensive if your blood pressure is above 130 over 80. Previous guidelines started hypertension at 140 over 90. This means an estimated 30 million Americans will qualify for the designation of having high blood pressure, and of those, an estimated 1 in 5 are likely to receive the recommendation to take blood pressure medication.
Flawed Fat Recommendations Have Been Followed With Disastrous Consequences
Since the 1950s, when vegetable oils began being promoted over saturated fats like butter, Americans have dutifully followed this advice, dramatically increasing consumption of vegetable oil. Soybean oil, for example, has risen by 600 percent while butter, tallow and lard consumption has been halved. We’ve also dramatically increased sugar consumption, which has also been implicated as a primary contributor to heart disease and other chronic health problems.10
While following this advice, Americans have gotten fatter and sicker. Heart disease rates have not improved even though people have been following the AHA’s “heart healthy diet.” Common sense tells us if the AHA’s advice hasn’t worked in the last 65 years, it’s not likely to start working now. Modern research is just now starting to reveal what actually happens at the molecular level when you consume vegetable oil and margarine, and it’s not good.
For example, Dr. Sanjoy Ghosh,11 a biologist at the University of British Columbia, has shown your mitochondria cannot easily use polyunsaturated fatty acids (PUFAs) for fuel due to the fats’ unique molecular structure. Other researchers have shown the PUFA linoleic acid hinders mitochondrial function and can even cause cell death.12
PUFAs are also not readily stored in subcutaneous fat. Instead, PUFAs tend to get deposited in your liver, where they contribute to fatty liver disease, and in your arteries, where they contribute to atherosclerosis.
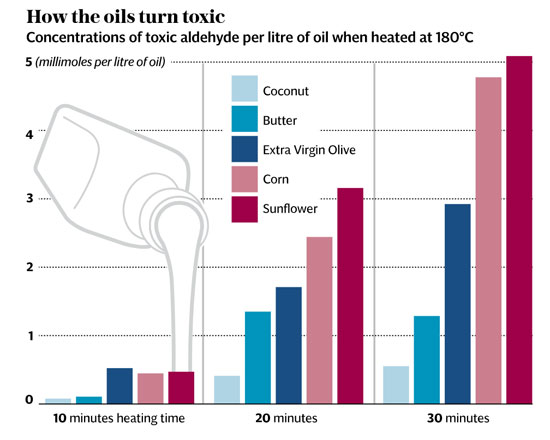
According to Frances Sladek,13 Ph.D., a toxicologist and professor of cell biology at UC Riverside, PUFAs behave like a toxin that builds up in tissues because your body cannot easily rid itself of it. Making matters worse, when vegetable oils like sunflower oil and corn oil are heated, cancer-causing chemicals like cyclic aldehydes are also produced.14
Vegetable Oils Are Anything But Healthy
Other research confirms such findings by linking fried foods to an increased risk of death. For example, eating fried potatoes more than twice a week has been shown to double a person’s risk of death compared to never eating fried potatoes.15 Animal and human research has also found vegetable oils promote:
- Obesity and fatty liver16
- Lethargy and prediabetic symptoms17
- Chronic pain/idiopathic pain syndromes (meaning pain with no discernible cause)18
- Migraines19
- Crohn’s disease and ulcerative colitis20
According to Dr. Cate Shanahan,21 a family physician and author of “Deep Nutrition: Why Your Genes Need Traditional Food,” the idea that PUFAs are healthier than saturated fats falls flat when you enter the field of biochemistry, because it’s “biochemically implausible.” In other words, the molecular structure of PUFA is such that it’s far more prone to react with oxygen, and these reactions disrupt cellular activity and cause inflammation.22 Oxidative stress and inflammation, in turn, are hallmarks not only of heart disease and heart attacks but of most chronic diseases.23,24
“[T]he folks at the AHA claim saturated fat is pro-inflammatory and causes arterial plaque and heart attacks — but there is no biochemically plausible explanation for their argument,” she told me in an emailed rebuttal to the AHA advisory. “Saturated fat is very stable, and will not react with oxygen the way PUFA fat does, not until the fundamental laws of the universe are altered.
Our bodies do need some PUFA fat, but we need it to come from food like walnuts and salmon or gently processed (as in cold pressed, unrefined) oils like flax and artisanal grapeseed, not from vegetable oils because these are refined, bleached and deodorized, and the PUFA fats are molecularly mangled into toxins our body cannot use.”
Open Letter to AHA President
In an open letter to AHA president Warner, Dr. William Davis, a New York cardiologist and author of The New York Times best seller “Wheat Belly, Lose the Wheat, Lose the Weight, and Find Your Path Back to Health,” writes, in part:
“If you ignore the nonsense that AHA policy dictates, you can absolutely gain control over cardiovascular risk. But you will NOT find the answers in any AHA policy. I learned these lessons practicing as an interventional cardiologist, then abandoning this ridiculous way of managing coronary disease to devote my efforts to early detection and prevention.
So, I thought I would articulate some of these thoughts in an open letter to Dr. Warner as he recovers from his procedure … Dr. Warner — … There are a number of reasons why someone like you — deeply-entrenched in the conventional world of heart disease management and what passes for prevention — highlights the miserable failure that the modern coronary care paradigm represents:
1) We are trapped by the outdated but profitable lipid hypothesis … 2) We know from abundant data that small oxidation- and glycation-prone LDL particles are highly atherogenic … are potent triggers of the inflammation cascade … and are triggered to abundant degrees in some genotypes upon consumption of the amylopectin A of grains …
[Y]es, the food that the American Heart Association advises to fill the diet with — and sugars … I am hoping that, now that this disease has touched you personally, your eyes will be opened to the corrupt and absurd policies of conventional coronary care and the American Heart Association.”
The Magic Pill Myth Needs to End
Davis goes on to note that heart disease is a multifactorial problem that cannot be solved with a pill.
“Thinking that a statin drug … [is] sufficient to prevent coronary events is absurd and overly-simplistic, like thinking that taking Aricept for dementia will stop the disease — of course, it does no such thing,” he writes, adding, “There are no drugs to ‘treat’ many of the contributors to coronary atherogenesis. But there are many non-drug strategies to identify, then correct, such causes.”
Nondrug prevention strategies suggested by Davis include:
• Avoiding any and all dietary factors that provoke insulin resistance, glycation and formation of small, dense LDL particles. Importantly, this would include avoiding the harmful fats recommended by the AHA such as margarine and processed vegetable oils, and keeping your total daily fructose consumption below 25 grams per day.
• Optimizing your vitamin D level.
• Optimizing your omega-3 fat intake: An omega-3 index of 10 percent or greater is associated with “dramatic reduction in cardiovascular events,” Davis notes. Indeed, a 2010 analysis25 found that while diets higher in omega-6 fats (found in ample amounts in vegetable oils) and lower in omega-3s increased the risk of nonfatal myocardial infarction and death from heart disease by 13 percent; a mixed diet of both omega-3 and omega-6 fats reduced these risks by 22 percent.
Meanwhile, the AHA recommends higher intakes of omega-6, saying26 “Aggregate data from randomized trials, case-control and cohort studies, and long-term animal feeding experiments indicate that the consumption of at least 5 percent to 10 percent of energy from omega-6 PUFAs reduces the risk of coronary heart disease relative to lower intakes.
The data also suggest that higher intakes appear to be safe and may be even more beneficial.”This statement runs counter to a large body of research suggesting the converse — specifically, that reducing omega-6 fats and increasing omega-3 is better for your heart.
• Addressing your thyroid function.
• Optimizing your gut microbiome to address dysbiosis caused by excess sugar, chlorinated and fluoridated water, and exposure to antibiotics, pesticides and common heartburn drugs.
https://articles.mercola.com/sites/articles/archive/2017/11/29/aha-president-suffers-heart-attack.aspx
